Good nutrition is important to everyone but crucial to those with disease-related malnutrition or recovering from surgery. The body will then be working extra hard to restore good health, thus increasing nutritional needs.
It is the role of your medical team to ensure that you are well nourished and not suffering from malnutrition (a condition resulting from the body not getting the right amount of vitamins, minerals, and other nutrients needed to maintain health). One method of assessment is the
“MUST” tool which determines presence or risk of developing malnutrition (
shown below). The tool uses a points system to assign the appropriate level of intervention and / or monitoring.
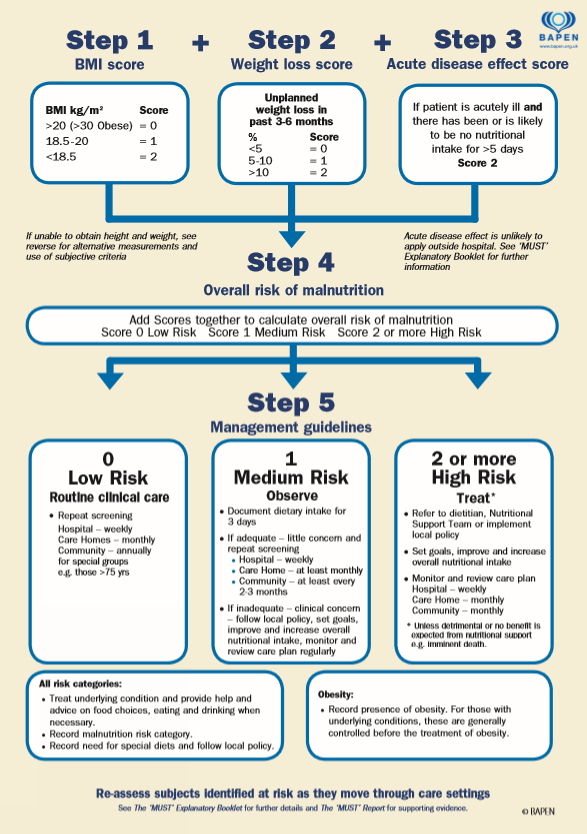 Malnutrution Universal Screening Tool, British Association of Parenteral and Enteral Nutrition (BAPEN)
Malnutrution Universal Screening Tool, British Association of Parenteral and Enteral Nutrition (BAPEN)
Once this has been determined your medical team is then required to ensure that you are able to meet your nutritional requirements and if not why this may be. For most people this can simply be achieved with a small increase or supplementation to their oral intake. However, if a patient has a problem with their digestive system and/or their condition results in an inability to fully meet their individual requirements for the essential nutrients it may be necessary to provide these in liquid form, through a tube.
These nutrients include carbohydrates, proteins, fats, vitamins, minerals and water; all essential to build body tissue and provide energy for bodily functions. Even an inability to fulfil your requirement for one of these has the ability to greatly affect your health.
You will be accessed to ensure that the type of tube feeding that is made available to you will be appropriate for you to maximise your nutritional intake. The diagram below illustrates how such decisions are made:
There are also different types of liquid feeds available, both for enteral and parenteral nutrition therapy and your dietitian will ensure that you receive the type specific to meet your requirements taking in to account all aspect of your medical history.
As you are monitored there may be times where feeds are changed, it may be to introduce/reduce calories, add/remove individual components, or alter feeding times and volumes. These are all to ensure you retain a healthy nutritional balance.
There will be a number of people involved with your nutritional care. Many hospitals have a 'Nutrition Team' who have constituent members; Consultant, nutrition nurse specialist, dietitian and pharmacist. Additional members may be a biochemist, speech and language therapist or a psychologist. Where there is no nutrition team you will have nominated healthcare professionals who will manage your care. You should always find out who and how to contact your nominated healthcare professionals when you have issues/questions/concerns in relation to your home artificial nutrition.